Vitamin D
On this very long page I would like to tell you in detail what I have learned about vitamin D after years of thorough study. But before I do that, I will first mention the prevailing opinions that you will encounter if you do a quick search:
Vitamin D is a fat-soluble vitamin that is needed to absorb calcium and phosphorus, for strong bones and teeth, good muscle function, the immune system, fertility, less fat storage and even against aging. It's the sun vitamin but our sun doesn't have enough power so we have to take it. If young children do not do this sufficiently, they will develop skeletal abnormalities or cancer later in life. The elderly suffer from osteoporosis or muscle weakness.
The vitamin traders promote high doses and proudly state that they successfully lobby government agencies for higher recommended amounts and maximum permitted doses. It seems to get crazier and crazier and I am always shocked by what I encounter.
The only thing that vitamin D devotees don't seem to agree on is how much of that miraculous vitamin is enough. Opinions differ on this matter and the division is so great that conferences are being organized to discuss the “controversies in vitamin D”.
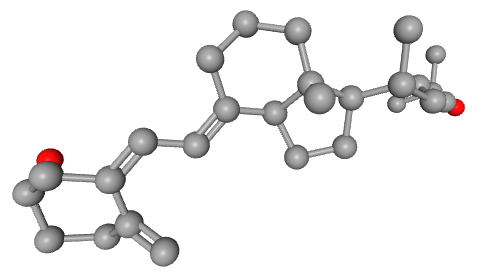
Oddly enough, everyone seems to agree that we produce vitamin D in our bodies with sunlight. We don't even need mushrooms or anything like that. You may be thinking: but if we produce it ourselves, then vitamin D isn't a vitamin! That's right. By definition, this secosteroid shouldn't be called a vitamin. We also produce the precursor, the substance from which it is formed, ourselves. But historically, it has happened that we now call this endogenous substance vitamin D, even though we are fully capable of producing the substance in our own bodies.
After more than a century of research, it is well known how exactly this production takes place. The page on cholesterol on the website of The Medical Biochemistry Page shows it very precisely. Below I have copied a small section from the image on that page with the cholesterol in the center. Cholesterol is also the raw material for bile and our steroid hormones. And we create all of these ourselves. This includes testosterone and estrogen. Vitamin D is sometimes also called a steroid hormone.
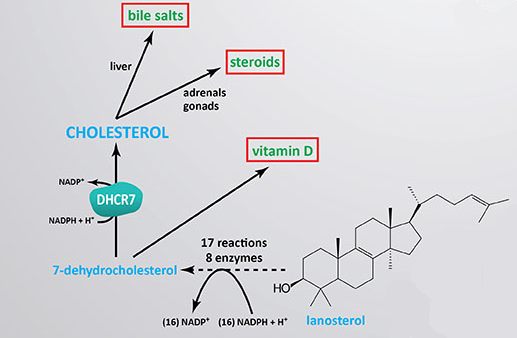
The picture shows that we make bile salts and hormones (“steroids”) from cholesterol. We produce vitamin D from the precursor of cholesterol, the substance 7-dehydrocholesterol. What we produce and do not use immediately, our body stores in the liver and in fatty tissue. This happens with other animals too. So when we eat animal products, we get a little extra through the fat from those animals. For example, via milk fat and eggs. And we store that little extra. Otherwise it would get in our way, because we have already produced it ourselves.
If a hormone accidentally comes along with that butter, cheese, eggs and other animal products, that does not mean that that hormone is a “nutrient”, a food. Our body will actually keep those extra hormonal substances out of the bloodstream, to remove them via the liver with the bile. That is what it does when we ingest such unwanted substances. Even if they are added or “supplemented” consciously and with the best intentions.
But how did we end up in this inverted reality? How is it that we have walked this path with the rest of the world for a whole century? Where was that wrong turn taken? Perhaps we can learn something if we dig into history.
The History
In the 19th and early 20th century there was much poverty and food shortages, which led to many deficiency diseases. Rickets is a bone disorder that mainly affects growing children. It was a prevalent deficiency disease for which no anti-factor or “vitamin” had yet been found. The obvious and well-known cause of rickets was, of course, the lack of food at the time. But that problem could not be solved quickly. It must have been an attractive idea to be able to combat the disease with a simple substance. Especially if a patent could be taken on its production. And lo and behold, it worked!
The well-known home remedy for all sorts of ailments was cod liver oil. Also for rickets. That was already the case in the 19th century. And also doctors started experimenting with it.
Infobox: cod liver oil as a remedy for rickets
Due to the prevailing poverty and food shortages, all sorts of “solutions” were sought. There was a lot of deceit. Everything was diluted and mixed with cheap substances that do not belong in food.
Infobox: the counterfeits with bread and flour
Growing children suffered from this poor nutrition. It was clear that rickets was not caused by a lack of squeezed-out livers from dead fish. But also doctors used the home remedy cod liver oil as a medicine in the treatment of rickets. They probably knew that these children simply did not get the nutrition they needed and it was mainly an emergency measure.
Infobox: the papers of Dr. Haakma Tresling and the idea of Dr. Kassowitz
For a long time, good nutrition remained difficult for people in poverty. That is why there was a lot of experimenting in the early 20th century in the search for that “silver bullet”, a vitamin! The experiments were done on animals and supplying laboratory animals became a specialism. Rats turned out to be the most suitable, because they are small and have a short life span.
These rats had to be specifically made suitable for the rickets experiments. This was done by simply not feeding them calcium. But not giving them phosphorus also worked. Without either or both of these elements they became rachitic. Or by giving these elements in a very skewed ratio. It was known that bones are built from calcium phosphate, a compound of lime and phosphorus. In short: it was well known at the beginning of the last century which nutritional deficiency causes the condition rickets!
Infobox: the rickets diet for growing animals
Around 1916 it became clear that light played a role and had effects comparable to those of cod liver oil. It was Harry Steenbock who discovered this in the goats he was experimenting on. He gave them rickets by not giving them enough calciumplugin-autotooltip__default plugin-autotooltip_bigSee Infobox above: "a low lime ration"; lime is calciumoxide.. He had noticed that in the summers the animals seemed less rachitic. 8)9)
Infobox: the effect of UV light on malnourished children and rats
It is likely that the UV light stimulated the production of vitamin D (cholecalciferol) in the malnourished animals and humans. Also direct intake of cholecalciferol “compensates” for the nutritional deficiency in rickets. But the cause of the condition rickets still remains that nutritional deficiency!
In 1922, Elmer McCollum—yes, the one with the scientific misconduct—proved the existence of a “calcium-depositing vitamin” by distinguishing this factor from the factor vitamin A. 13)
In the frenzy of the day, and with the letters A, B and C already in use, the new vitamin was subsequently named vitamin D. To provide his proof, McCollum conducted experiments on rats, which he put on a calcium-poor diet to give them rickets.
Infobox: the evidence of McCollum and his malnourished rats
This historic experiment by McCollum also shows that rickets is caused by malnutrition. And that an “anti-rickets factor” can “compensate” for malnutrition to a certain extent, “with greater efficiency”. That “anti-rickets factor” was different from the already known “growth factor” vitamin A. That distinction was perhaps a valuable discovery.
Meanwhile, Edward Mellanby eventually found that oatmeal porridge was the most harmful variant of the one-sided diets for his puppies. He was most successful in causing rickets in dogs with this diet. Oats have the worst calcium/phosphorus ratio of all grains.
Infobox: Mellanby on oatmeal in 1925
Also McCollum was still looking for “well-working” diets that consistently caused rickets. But that wasn't easy: unexpectedly the rats stopped getting rickets. And it wasn't because they had been getting vitamin D in their diet!
Infobox: McCollum on the setback he encountered in 1925
In the same year, 1925, the process was started to patent the production of vitamin D. In 1927 Quaker Oats obtained the first license to exploit the method of Harry Steenbock. 16) Philips in Eindhoven, Holland concluded an agreement with chocolate manufacturer Van Houten in Weesp (1930). In 1931 the chocolate lozenge with the anti-rachiticum was patented and marketed under the name Dohyfral. In 1937 Philips-Van Houten signed a licensing agreement with DuPont de Nemours. The large American chicken farms in particular were major customers. 17)
It was the start of a billion-dollar industry. However, researchers at the time understood very well that while vitamin D could be called an “anti-rachitic”, rickets could not be caused by a lack of vitamin D. The anti-rachitic agent was only anti-rachitic in cases of severe malnutrition. From 1934:
The rachitic condition in the rat cannot be brought about by a deficiency of vitamin D alone. A rachitogenic diet must also be grossly abnormal in the proportion of its mineral constituents in order to produce a good degree of rickets. 18)
We know that indeed the calcium/phosphorus ratio is important. That ratio must be greater than 1, so more calcium than phosphorus. However, for grains such as wheat and especially oats, this ratio is reversed. Oats are notorious among horse lovers. Mellanby indeed found that oatmeal porridge was the most harmful cereal porridge.
This disturbed ratio is primarily necessary as a cause of rickets, only then does the addition or not of the hormonal substance “vitamin D” make a difference. In 1941 Thomas Moore formulated it as follows:
In the case of vitamin D a derangement of the calcium to phosphorus ratio of the diet is necessary, as well as a deficiency of the vitamin, for the development of rickets. 19)
But can the absence of that medicine, the anti-rachitic vitamin D, really be called a “deficiency” if the real cause is a disturbance of the calcium-phosphorus ratio in the diet? As the physician Theunis Haakma Tresling wrote in 1860, the diet should be put in order first. Then there is no need to “compensate” with added vitamin D, which we now know is much more of a hormone than a vitamin.
Infobox: Anthony Norman on vitamin D
We have been fooling ourselves, aided by the half-truths of a vitamin industry, the leading “cash cow” of the pharmaceutical companies. 22) We all really wanted to believe it. Because who wouldn’t want a miracle cure that helps with everything and anything and that doesn’t even require you to eat healthily? We wanted very much that miraculous vitamin that ensures strong bones and much more. But that miracle does not exist. It turns out not to be true. Yes, in severe malnutrition the steroid hormone vitamin D works wonders by skewing the system. At what expense? And rickets did not disappear thanks to the addition of vitamin D to our daily diet. The cause of rickets was the prevailing food shortage.
What do we actually know about the side effects of this drug? Are there any in the long term? What side effects could “compensating” with that steroid have?
Covert Poisoning
For bone formation, the diet must provide sufficient calcium and phosphate, in a reasonable ratio. And a well-functioning vitamin D metabolism is necessary to subsequently absorb the calcium and phosphorus into the bone tissue. 23)
The body produces all the vitamin D required for the metabolism from cholesterol. This will not work any better if we take extra of that metabolite, that regulating substance. Our bodies can arrange this very well on their own. More is not better.
Infobox: taking vitamin D is unnecessary and counterproductive
Taking vitamin D disrupts the proper functioning of the vitamin D metabolism and throws it out of balance. This has a direct effect on the calcium balance. Calcium is important for many more processes than bone formation. Blood clotting and the proper functioning of muscles and nerves also depend on it. The calcium level in the blood is tightly regulated.
Excessive intake of vitamin D leads to calcifications, such as kidney stones. 27) This regulation can even be disrupted to such an extent that the calcifications lead to “system failure”. You can die from it:
If calcium levels in blood rise too much too rapidly, and the normal regulation by hormone activity fails to counteract the process, the net result is a system failure responsible for resulting calcification diseases including blockage of the circulatory system. 28)
Vitamin D has been used commercially since the 1980s as an effective means of combating rats, after conventional rodenticides were no longer adequate. 29)30)
But vitamin D can also be fatal for humans. This boy, this baby and this and this man all died from it in recent years.
Endogenous Production
The great thing is that our body will never produce too much vitamin D and harm itself. Not even if you sit in the sun for a very long time. Because then that same sunlight ensures that the surplus in the skin is immediately broken down.
Therefore no matter how much sun a human is exposed to vitamin D intoxication will not occur because any excess previtamin D3 and vitamin D3 is photodegraded into products that have no calcemic activity. 31)32)33)
But even without the sun, the D metabolism continues to work fine. In fact, not only is there no evidence that we should take vitamin D, there is even no evidence that we need (ultraviolet) light to produce it ourselves.
Two Routes
There are two ways in which we can obtain this important, endogenous substance vitamin D:
- by producing it ourselves from a cholesterol precursor (7-dehydrocholesterol) with energy such as in light (UVB),
- by consuming animal products, or supplements with cholecalciferol (vitamin D3plugin-autotooltip__default plugin-autotooltip_bigvitamin D2, or ergocalciferol, from fungi is a non-animal source and there are also plants with D3).
In the first way, we provide ourselves with the vitamin D we need in a safe and effective way. An adequate amount is produced in the skin under the influence of light energy. The light, to which the vitamin D itself is also exposed via the skin, ensures that an excess is immediately broken down again. In this way production is limited.
The second route, direct and via the intestines, is riskier. In this way, the limited endogenous production is circumvented. An excess can only be stored away. This occurs in the liver and in fatty tissue. An excess will persist for a long time and will only be removed slowly, with a half-life of about two months. Ultimately, this will not only disrupt the calcium balance, but can also hinder the gene expression. 36) Vitamin D intoxication can occur insidiously or acutely, and is difficult to treat.
Cholecalciferol has a very narrow margin of safety, which means that even small ingestion of this poison can result in severe clinical signs or death. Toxic ingestions must be treated quickly and appropriately to prevent kidney failure. 37)
The Metabolism
The miracle drug vitamin D was discovered in the 1920s. It was supposed to ensure healthy and strong bones and much more. But a hundred years later, little is noticeable and it seems as if people become increasingly ill the more they take of this vitamin. In 2008, Anthony Norman expressed his concerns about the lack of health benefits in The American Journal of Clinical Nutrition:
Despite many publications and scientific meetings reporting advances in vitamin D science, a disturbing realization is growing that the newer scientific and clinical knowledge is not being translated into better human health. 38)
What could possibly go wrong here? If an 'engineer' were to ask that question, he would look at how the system works. And that is exactly what Trevor Marshall did in 2008. He mapped out the vitamin D metabolism, with all the mechanisms and feedback loops as they were known at the time.
The model we have elucidated for the D metabolism is complex, but not particularly so. 39)
Regulated System
In the Infobox below I am happy to explain the details of that metabolism and Marshall's findings. It is a complex model, but easy to follow if you take the time and sit down for it. I find it fascinating because it explains where things go wrong in diagnosing that much-dreaded “vitamin D deficiency”. Marshall shows that vitamin D metabolism is an elegantly working regulatory system. He also shows that, within that system, it is only logical that our body will adjust the 25-D (your “vitamin D value”) itself when necessary.
Infobox: vitamin D metabolism is a regulatory system
Marshall's suspicion from 2008 has now been confirmed. Research shows that disease processes indeed downregulate the value of 25-D, the blood value which is measured during a vitamin D test.
Cause or Effect?
The clinical vitamin D determination is not based on the actual concentration of vitamin D in the blood. Such a test is not available and will not be available anytime soonplugin-autotooltip__default plugin-autotooltip_big"Furthermore, researchers are unlikely to develop a routine serum vitamin D clinical assay in the future.". 42) No, the vitamin D value that the lab determines is the measured value of 25-D. In many chronic diseases, that value appears to be relatively low, the well-known “vitamin D deficiency”. 43) Marshall writes about this:
What developed has been a concept of ‘Vitamin D Deficiency’ based solely on the assumption that ‘low’ Vitamin D serum levels somehow cause disease processes.
It is assumed that the conversion to 25-D is not regulated and that its specific value is indicative of the concentration of vitamin D. 44) However, in 2019, a number of studies were published that showed that in obese mice the concentration of 25-D does indeed vary and appears to be regulated by disease processes. In diabetes too, 25-D appears not to be produced stably.
Infobox: the downregulation of 25-D in the event of illness
It appears that the low values of 25-D found in illness are caused by that illness and are the logical effect of a control system. That would mean the end of a dogma, because it is dogmatically assumed that the low values found in illness are a “deficiency” and that this must be supplemented. But if the body itself downregulates that 25-D out of necessity, then “supplementation” would only frustrate that regulation process.
Cum hoc ergo propter hoc is a classic fallacy. Correlation does not imply causation. The low 25-D levels are indeed always seen in obesity, but that does not mean that the “low vitamin D level” causes obesity. Let alone that obesity will disappear by taking vitamin D. This non-sequitur will not be the last dogma to be abandoned.
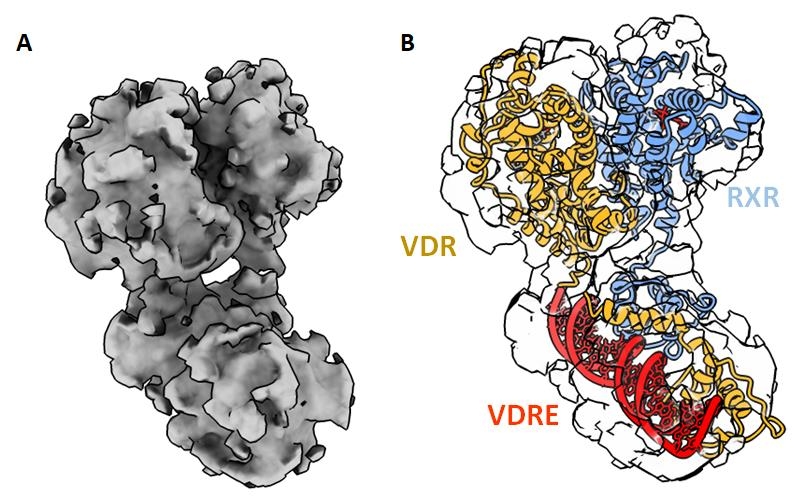
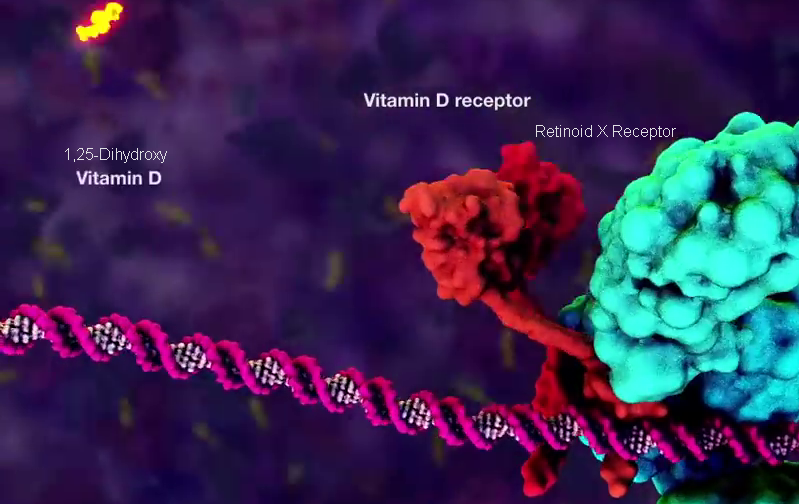
Transcriptional Activation
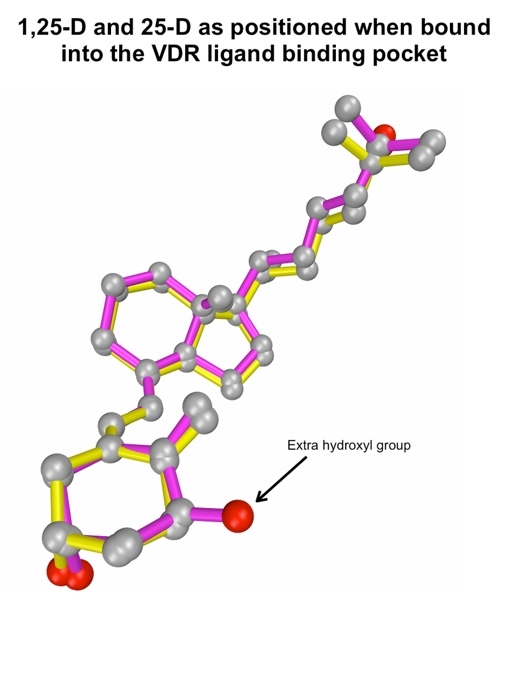
It was not until the late 1980s that the structure and function of the “Vitamin D Receptor” (VDR) was determined. 50)51) This demonstrated that vitamin D metabolism plays a very important role in the expression of our hereditary material, or gene expression. We now know of more than 900 proteins for which the activating metabolite is required in that vitamin D metabolism. Many of these proteins are involved in the formation of bones and teeth, but a properly functioning vitamin D system is also required for the production of many immune substances. The substance, or metabolite, that initiates gene expression in our cells, i.e. activates the transcription of genes into proteins, is 1,25-D (also called calcitriol, or 1,25-dihydroxyvitamin D).
Infobox: activating or blocking the receptor
If the concentration of the precursor metabolite 25-D is now increased, it will become more difficult to activate the receptor with 1,25-D. The increased 25-D will then hinder transcription and fewer proteins will be produced. Increasing the “vitamin D level” 25-D disrupts gene expression, the function of the vitamin D receptor. The more disruption, the less gene expression and the fewer of the proteins required by the cell are produced. Fewer bone-forming building blocks and fewer enzymes, for example. But also fewer immune substances, such as all kinds of antimicrobial peptides, the body's own antibiotics. 57)
This immunosuppression could explain the popularity of vitamin D. After all, suppressing immune responses reduces the severity of various symptoms in chronic conditions. You might think of vitamin D as an over-the-counter steroid hormone and immune suppressants. Taking vitamin D does indeed suppress the immune system, which means it can be used therapeutically in so-called autoimmune diseases: 58)
Vitamin D has multiple immunosuppressant properties.
On the whole, vitamin D confers an immunosuppressive effect.
Moreover, recent evidence strongly suggests that vitamin D supplementation may be therapeutically beneficial, particularly for Th1-mediated autoimmune disorders.
Other proteins will also be produced less with increased vitamin D intake, such as those for bone formation and teeth formation. If the level is very high, this is called hypervitaminosis, vitamin D poisoning. At a young age, this can have serious consequences for early development.
Infobox: disrupted tooth formation due to excessive vitamin D intake at a young age
At least 913 genes have been recognized for known proteins that require activation of the VDR. 65) Disrupting gene expression, the function of the vitamin D receptor, can therefore lead to a wide variety of diseases.
VDR and its ligand play important roles in calcium metabolism, cell growth, differentiation, antiproliferation, apoptosis, and adaptive/innate immune responses. VDR is a promiscuous NR, found in the prostate, ovary, breast, and the skin, and also in the brain, heart, pancreas, kidney, intestine, and the colon. Consequently, deregulation of VDR function may lead to severe diseases such as cancers, psoriasis, rickets, renal osteodystrophy and autoimmunity (multiple sclerosis, rheumatoid arthritis, inflammatory bowel diseases, type I diabetes. 66)67)68)
Ironically and sadly, vitamin D is taken precisely because it is supposed to help (“may be therapeutically beneficial”) with all of these conditions. Trevor Marshall on the urgent need for rethinking in his 2008 essay:
It is critical that Medicine revisits the role which has been assigned to “The Sunshine Vitamin,” properly recognizing its function as a secosteroid, a transcriptional activator, key to the proper operation of the innate immune system. 69)
Wonderful Machine
Infobox: vitamin A and vitamin D both influence the immune system
Finally, with the video below from WEHI TV, I would like to show you how beautifully the entire gene-expressing transcription machine functions. This happens in our bodies all the time, day and night, 24×7. We shouldn't want to disrupt that!
[PMID: 794773] [DOI: 10.1111/j.1753-4887.1976.tb05815.x]
[PMID: 21313221] [PMCID: 2477523] [DOI: 10.1136/pgmj.17.185.52]
[PMID: 16927375] [DOI: 10.1002/jcb.21031]
[PMID: 23183289] [DOI: 10.1159/000343104]
[PMID: 24166866] [DOI: 10.1002/jbmr.2121]
[PMID: 9245225] [DOI: 10.7326/0003-4819-127-3-199708010-00004]
[PMID: 29562593] [PMCID: 5872784] [DOI: 10.3390/nu10030366]
[PMID: 24494042] [PMCID: 3897598] [DOI: 10.4161/derm.24494]
[PMID: 8092101] [DOI: 10.1093/ajcn/60.4.619]
[PMID: 6256855] [DOI: 10.1126/science.6256855]
[PMID: 9675700] [DOI: 10.3177/jnsv.44.195]
[PMID: 18689389] [DOI: 10.1093/ajcn/88.2.491S]
[PMID: 18200565] [DOI: 10.1002/bies.20708]
[PMID: 17368181] [DOI: 10.1016/j.jsbmb.2006.12.038]
[PMID: 18695076] [PMCID: 2677029] [DOI: 10.1001/archinte.168.15.1629]
[PMID: 26681795] [PMCID: 4839493] [DOI: 10.1152/physrev.00014.2015]
[PMID: 30790351] [PMCID: 6663580] [DOI: 10.1002/jbmr.3686]
[PMID: 30833469] [PMCID: 6477896] [DOI: 10.2337/db18-1050]
[PMID: 2829212] [PMCID: 279689] [DOI: 10.1073/pnas.85.4.1005]
[PMID: 15322146] [DOI: 10.4049/jimmunol.173.5.2909]
[PMID: 17557889] [PMCID: 1955167] [DOI: 10.1136/ard.2007.069831]