Table of Contents

Vitamin Gold Rush
Before we look at vitamin A and vitamin D, it is good to first ask ourselves what exactly a vitamin is. Or rather, what it should be. The term 'vitamin' was coined in 1912 and has been very valuable for the acceptance of a new idea at the time, namely that food is more than just proteins, carbohydrates and fats. It was a Dutchman who provided proof for this revolutionary idea. Gerrit Grijns showed that for the digestion of carbohydrates from rice (the starch from the grain) a minute amount of a substance from the husks was also needed. This substance could prevent the tropical disease beriberi and was therefore called the anti-beriberi factor. It was the first in a series of “factors” of associated deficiency diseases. In a short time, a feverish search for even more of these – potentially very lucrative – factors began.
Infobox: the discovery of the vitamin
Ultimately it was decided to designate vitamins with letters. The anti-beriberi substance would henceforth be called vitamin B. We now know it as vitamin B1, because it turned out that a whole complex of substances played a role. The numbered B vitamins are mainly cofactors that are needed for all kinds of enzymes. That role explains why so minutely little of a vitamin is needed; after all, the enzymes themselves do not participate in the metabolic reactions. They are not used up. And the peels contain so little that hundreds of kilos of it were needed to isolate that one substance, that first discovered vitamin!
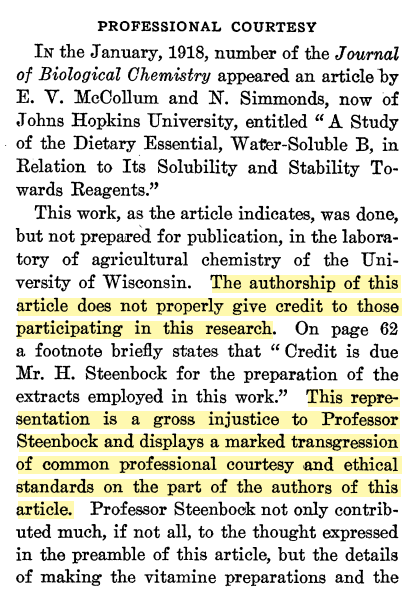
It was also in 1912 that Norwegian researchers discovered that the disease scurvy was probably caused by the lack of an anti-scurvy substance. We now know that substance as vitamin C or ascorbic acid. Isn't it remarkable that the first two vitamins discovered do not bear the first letters of the alphabet? This is thanks to the inventor of the vitamin alphabet, Elmer McCollum. He claimed the first letter as his own and also the discovery of vitamin A. The letters B and C were for the already discovered water-soluble vitamins, while vitamin A was fat-soluble. Later he discovered a second “fat-soluble vitamin” and logically that became vitamin D. A hundred years later his behavior still raises questions. The journey of discovery of vitamins was probably less beautiful than it is often portrayed.
Powerful Term
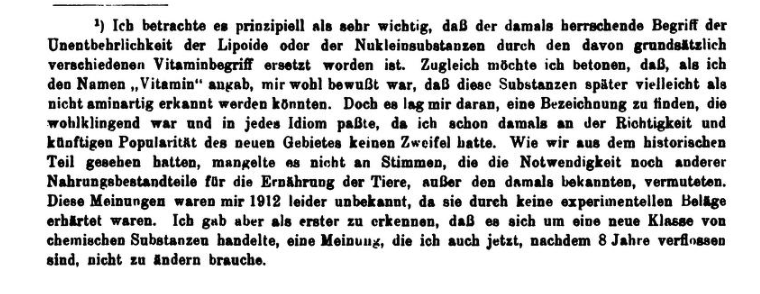
In the famous article from 1912, Casimir Funk first posits the term “vitamine”. In the article, Funk discusses the diseases beriberi, scurvy and pellagra. Three common diseases that seemed to be deficiency diseases. There was a lot of searching for the missing substances that would cause the respective diseases. In his article, Funk also mentions rachitis as a possible deficiency disease and encourages vitamin experiments to investigate this. He does mention that far too little is known about the enzymes and hormones that most likely originate from vitamins: 6)
I think that experiments with vitamins, which can at least do no harm, ought to be performed here in order to ascertain if a deficiency of the latter is not the real primary cause of the disease.
It is obvious that the minute amount necessary cannot be considered from the point of view of food. It is most probable that they are used as such or transformed into substances which are able to act in small quantities.
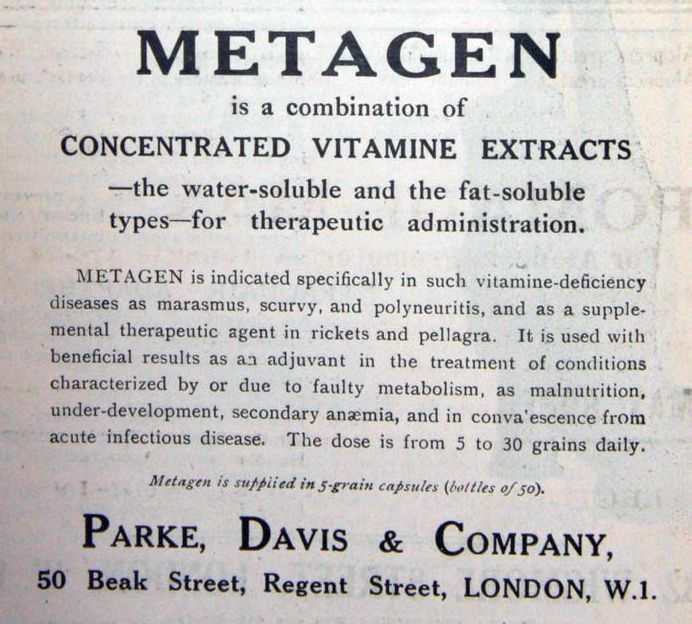
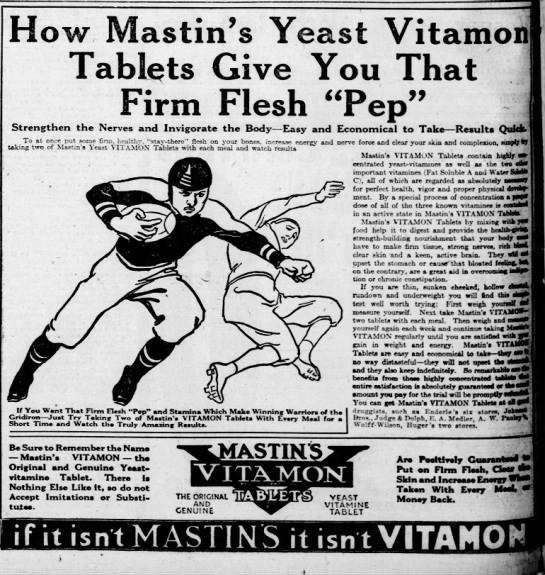
When Casimir Funk proposed the term “vitamine” in his scientific publication of 1912, he was looking for a term that sounded good and would suit everyone. The term may not have been entirely correct (because no “amines” were found) but it helped to accept the idea of deficiency diseases. It also helped create a rapidly growing vitamin industry unencumbered by regulation.
Infobox: successful marketing thanks to Casimir Funk
The term seems to have lost none of its power and is inextricably linked to health and vitality.
The Definition
With his term “vitamine”, Funk clearly referred to the micro-nutrient itself and not to the enzyme or hormone produced by the body for which that vitamin is needed. In 1970, neuroscientist and Nobel Prize winner 9) Paul Greengard defined a vitamin as follows:
A vitamin may be broadly defined as a substance that is essential for the maintenance of normal metabolic functions but is not synthesized in the body and, therefore, must be furnished from an exogenous source. 10)
Infobox: the statements of Paul Greengard
With the knowledge we have now, we must conclude that vitamin A and vitamin D are not in line with Funk's intentions, nor do they meet Greengard's definition. They are both substances that are produced by the body itself. For vitamin A, it turned out a few years after its discovery that the substance that does meet the definition is vegetable carotene.
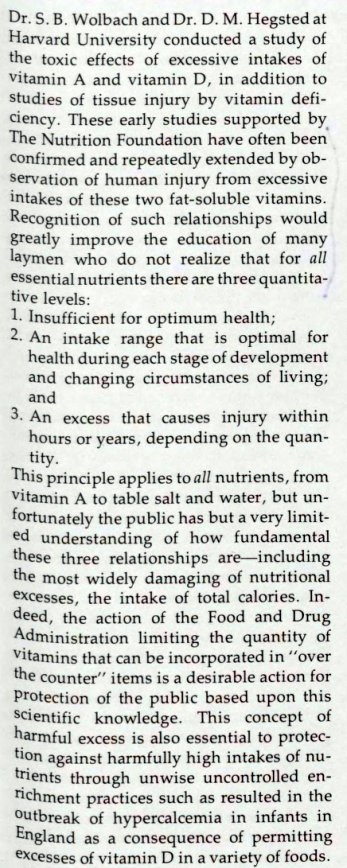
Furthermore, both retinol (vitamin Aplugin-autotooltip__default plugin-autotooltip_bigThe term "vitamin A" is often used for the group of substances from that metabolism, the vitamin A metabolism. On this site, vitamin A always refers to the substance retinol.) and cholecalciferol (vitamin Dplugin-autotooltip__default plugin-autotooltip_bigThe term "vitamin D" is often used for the group of substances from that metabolism, the vitamin D metabolism. On this site, vitamin D always refers to the substance cholecalciferol.) are part of internal regulatory systems. These systems ensure that the body's own production is limited. However, if these substances are added excessively from outside, via the diet or by “supplementation”, the regulatory systems that limit the body's own production are bypassed and blood values can become too high.
In addition, the determination of the blood value for vitamin D is based on an incorrect assumption. Instead of measuring the concentration of vitamin D in the blood, a derivative is determined, namely the value of the substance 25-hydroxyvitamin D (25-D). It is assumed that this value is a measure of the actual vitamin D in the blood. A direct clinical vitamin D determination (of cholecalciferol) is not available. However, the concentration of 25-D does not have a one-to-one relationship with that of vitamin D. It is therefore not a certain reflection of vitamin D in the blood. Studies have shown that the value of 25-D can be regulated by disease processes. If this happens, it gives a false impression of a “deficiency”. 11)12)
Vitamin A and vitamin D are both highly toxic. As early as the 1920s, when the substances were discovered, researchers warned of their deadly dangers in cod liver oil (see box). This oil from fish livers was always used by them in their research into the two fat-soluble vitamins. It was not until around 1930 that it became clear that plant carotene was the actual essential substance from which retinol (vitamin A), as found in the livers, is formed. It had already been discovered earlier that cholecalciferol (vitamin D) is formed by the body itself, under the influence of sunlight.
Interests and Standards
In 1929, Thomas Moore wrote in the leading journal The Lancet that - very likely - carotene from carrots is converted into vitamin A by the laboratory animal. In 1930, another report from Moore followed in which he confirmed his discovery. 15)16)
You may now be thinking: great, the real vitamin had been found! And the use of the toxic livers from cadavers was a mistake. Better to turn back halfway than to go completely astray! That's how it seemed to go at first. But what eventually followed was a 180-degree turn.
In 1931, the standards for vitamin A and vitamin D were established. This was important for trade and industry, for example to be able to assess vitamin preparations. The standard for vitamin A was then based on the safe carotene, the plant precursor. The substance ergosterol was assumed to be the plant precursor of vitamin D. Ergosterol was chosen as the standard for vitamin D.
This remained the case until after the Second World War, when the newly established World Health Organization took over the task of standardization. Since then, the standards have been based on the body's own endogenous substances, the toxicity of which had already been established in the 1920s and confirmed again and again. A remarkable twist. In the early 1940s, the issuing of recommended intakes had already begun, in which “safe dosages” were laid down.
Genetic Disruptions
From the 1970s onwards, research into vitamin A and vitamin D took some unexpected turns. It turned out that many more substances were involved in these metabolisms; for both vitamin A and vitamin D, a series of different metabolites appeared to provide the final effect. Then the signaling effect also came as a surprise: it meant that there was suddenly talk of steroid and retinoid hormones. 23)24)25)26)
But eventually it was discovered that vitamin A and vitamin D both play a crucial role in gene expression, translating our hereditary material into the corresponding proteins. For example, the building blocks for the skeleton, or enzymes, or antibodies. Disrupting that genetic system can have far-reaching consequences. A disruption during embryonic development gives rise to the risk of birth defects. Disruptions during growth and early development pose a risk of abnormalities in, for example, the musculoskeletal system or teeth. Later in life, a disrupted system can lead to all kinds of different chronic and immune diseases. More than 500 target genes have been found for vitamin A. For vitamin D at least 913 have been identified, but possibly even thousands. Both vitamins are inextricably involved in gene expression. 27)28)29)30)
At the end of the 20th century, vitamins A and D turned out to work very differently than previously assumed. The vitamin A and vitamin D puzzle turned out to be much more complex than it seemed a century earlier.
[PMID: 23798047] [DOI: 10.1024/0300-9831/a000123]
[PMID: 1095967] [DOI: 10.1111/j.1753-4887.1975.tb05095.x]
[PMID: 16744164] [PMCID: 1252282] [DOI: 10.1042/bj0221461]
[PMID: 13199651] [PMCID: 2542188]
[PMID: 31794861] [PMCID: 7987234] [DOI: 10.1016/j.bbalip.2019.158580]
[PMID: 35245207] [PMCID: 9066576] [DOI: 10.1530/EC-21-0594]
[PMID: 18689389] [DOI: 10.1093/ajcn/88.2.491S]
[PMID: 8227879] [DOI: 10.1016/0002-8223(93)91956-q]